Hamstrings: Cohesive group or frenemies?
The human body's musculoskeletal system creates movement in amazing ways. Regardless of what you are doing, your body’s goal is to create a relationship between stability, strength, and mobility. We achieve this harmony through a series of subsystems; a subsystem being a series of muscles from head to toe that are linked via fascia, common bony anchors, and neural connections. Among these, the Deep Longitudinal Subsystem (DLS) and the Intrinsic Stabilization Subsystem (ISS) play critical roles. This article will look at how these two parts work together, focusing on three muscles: the biceps femoris, semitendinosus, and semimembranosus. We'll see how they affect our ability to move powerfully and efficiently.
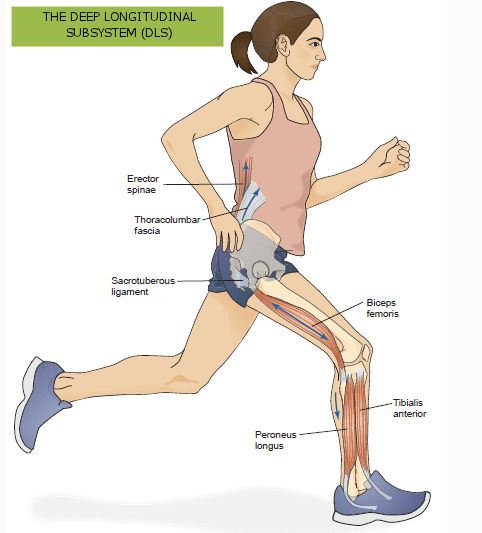
Understanding the Deep Longitudinal Subsystem (DLS)
The DLS is a key player in how we move. It includes several important parts of our body, like the thoracolumbar fascia, erector spinae, rhomboids, sacrotuberous ligament, and muscles in our lower legs. The DLS helps coordinate movement between our upper and lower body, especially during activities that involve our hips, lower back, and spine. In particular, during normal walk cycles, the DLS controls our leg swing and provides the driving force for forward propulsion.
As you become familiar with the location of the DLS, note it’s path towards the lateral side of the thigh and leg. Think about how- in the event of a muscle contraction- this would bias movement towards abduction (away from the midline) or external rotation. Bear that in mind when we start talking about the Intrinsic system!
Role of the Biceps Femoris
The biceps femoris is a major muscle in the DLS. It runs from our pelvis to our lower leg and is important for bending our knee and moving our hip. This muscle also helps keep our knee stable and helps control our pelvis when we walk or run. The most common dysfunctional pattern of the biceps femoris is to be overactive and often- though not always!- tight.
THE Intrinsic Stabilization Subsystem (ISS)
Unlike the DLS, the ISS is all about providing stability to our body. It's made up of deeper muscles like the multifidus, transversus abdominis, diaphragm, and muscles in our pelvic floor. The ISS keeps our lower back and hips stable, controls our movements, and helps prevent injuries.
It is critical to understand that these muscles generate little to no movement. Their role is to create stability- a strong base from which all movement can occur.
Semitendinosus and Semimembranosus: A Closer Look
The semitendinosus and semimembranosus, like the biceps femoris, originate from the ischial tuberosity and insert onto the tibia. They play roles in knee flexion, hip extension, and internal rotation of the tibia. They also have a significant impact on pelvic stability, a function closely tied to the ISS.
Interaction Between DLS and ISS
The DLS and ISS balance each other out. While the DLS is more about moving and creating force, the ISS provides a stable foundation for these movements. This balance is really clear when we look at how the biceps femoris works with the semitendinosus and semimembranosus, which are part of our hamstring muscles. Recall that the biceps femoris has an influence on external rotation. So, although the biceps femoris is grouped with the semitendinosus and the semimembranosus as the collective “hamstrings”, they have a few opposing roles! Certainly, they all work together to flex the knee, but that flexion can be torqued by an uneven pull of the muscles.
The most common thing we see is when someone has a “weak core” and knee pain during running and/or squats. At Ascend PT we often assess your squat to parse out the interaction of your subsystems. What we often see is:
Feet turning out.
Knees collapsing in with feet overpronating OR knees spreading apart with feet oversupinating (the big toe will sometimes leave the ground)
Anteriorly tilting pelvis.
Torso leaning forward too far.
Overcompensation and Power Transfer
When you show the squat pattern described above, the next step is to put you on the examination table where we investigate your core activation, hamstring length, and hip mobility (among other things). What we find is:
Weak “inner unit”. The Transverse abdominis and internal obliques are inhibited or weak.
Short range of motion in an active straight leg raise BUT full range of motion in an passive straight leg raise. If you can’t stabilize your pelvis as you lift your leg, it will shift into an anterior pelvic tilt. This creates tension on the hamstring group thus appearing “short and tight”. BUT if the therapist moves your leg, the hamstrings are allowed to show their full range.
Weak semitendonisus and semimembranosus BUT strong biceps femoris. Often times, as we test the biceps femoris, the patient’s back will “feel tight” as well.
Internal rotation of the tibia is limited, external rotation is full if not excessive.
Addressing Overcompensation
Correcting overcompensation involves a multifaceted approach:
1. Strengthening the ISS: Enhancing the strength and function of the intrinsic stabilizers, particularly those supporting the lumbar-pelvic-hip complex, is crucial. This can involve exercises targeting the deep abdominal muscles, multifidus, and pelvic floor.
2. Release the biceps femoris: It’s a bit counterintuitive, but sometimes a muscle can be long and overactive. For folks who have an anterior pelvic tilt, they have plenty of length in their biceps femoris, but they recruit it so much that it feels very tight. In this case, a seated “pin and stretch” technique will help to reduce recruitment without creating even more length.
3. Activate the medial hamstrings: To do this, you’ll take any knee flexion exercise and turn your toes in. In the example below, we use a standing hamstring curl but rotate the foot inwards. This biases the medial hamstrings because of their attachment site. Be prepared to feel VERY weak here- don’t be surprised if you have to go down in weight by a lot!
4. Put it all together: During your squats, the trick is to find the ball of the foot at the base of the big toe. If you can keep it firmly planted into the floor while also keep the knees in line with the foot- if not pressed apart slightly- you will find that your squat is able to drop deeper and press out harder. You may also find that there is a greater sense of stability, more core recruitment, and less tension in your back.
IN CONCLUSION
The interaction between the Deep Longitudinal Subsystem and the Intrinsic Stabilization Subsystem, particularly the interplay of the biceps femoris with the semitendinosus and semimembranosus, is complex yet crucial for efficient body mechanics. Understanding this relationship and addressing overcompensation through a holistic approach can lead to improved functional performance, reduced injury risk, and better overall musculoskeletal health.
REFERENCES
Schleip R, Müller DG. Training principles for fascial connective tissues: Scientific foundation and suggested practical applications. J Bodyw Mov Ther. 2013;17(1):103-115. doi:10.1016/j.jbmt.2012.06.007
Janda V. Muscles, central nervous motor regulation and back problems. In: Korr IM, ed. The Neurobiologic Mechanisms in Manipulative Therapy. New York, NY: Plenum Press; 1983:27-41.
Bergmark A. Stability of the lumbar spine. A study in mechanical engineering. Acta Orthop Scand Suppl. 1989;230:1-54. doi:10.3109/17453678909154177
Hodges PW, Richardson CA. Inefficient muscular stabilization of the lumbar spine associated with low back pain: A motor control evaluation of transversus abdominis. Spine. 1996;21(22):2640-2650. doi:10.1097/00007632-199611150-00014
Neumann DA. Kinesiology of the Musculoskeletal System: Foundations for Rehabilitation. St. Louis, MO: Mosby; 2010.
Sahrmann SA. Diagnosis and Treatment of Movement Impairment Syndromes. St. Louis, MO: Mosby; 2002.
Chaitow L, Delany J. Clinical Application of Neuromuscular Techniques: The Lower Body. Volume 2. Edinburgh: Churchill Livingstone; 2008.
Liebenson C. Rehabilitation of the Spine: A Practitioner's Manual. Baltimore, MD: Lippincott Williams & Wilkins; 2007.
McGill SM. Low Back Disorders: Evidence-Based Prevention and Rehabilitation. Champaign, IL: Human Kinetics; 2007.
Cook G, Burton L, Hoogenboom BJ. Pre-Participation Screening: The Use of Fundamental Movements as an Assessment of Function - Part 1. N Am J Sports Phys Ther. 2006;1(2):62-72.
Brookbush Institute. Biceps Femoris. Brookbush Institute website. Accessed 11/01/2023. Available from: https://brookbushinstitute.com/courses/biceps-femoris.